Polycystic Ovarian Syndrome, or PCOS, affects 1.4 million women in Canada. It’s the most common endocrine disorder experienced by women of childbearing age. Although no specific cause has been identified, it always exists alongside a hormonal imbalance. Whether you’ve suspected that you have PCOS, or are looking for more clarity on how to manage symptoms, you’re in the right place.
How do you know if you have PCOS?
If you experience a combination of these symptoms, you may have PCOS:
- Irregular or absent periods
- Acne
- Thinning hair
- Hair growth on the face, chest or back
- Oily skin
- Struggles with fertility
- Polycystic ovaries
- Unexplained weight gain
Although these symptoms are often used to diagnose PCOS, more than half of those with PCOS don’t have any symptoms at all. In fact, some don’t discover they have PCOS until they have difficulty getting pregnant.
What causes PCOS?
There is no known cause for PCOS, but there are certain factors that increase the chances of it developing. The most common is insulin resistance, but heredity, environment, inflammation, and adrenal function all play a part in increasing the risk of developing PCOS.
Hormonal imbalance
Those with PCOS tend to have increased levels of androgens. Androgens are produced by the ovaries and adrenal glands, and include hormones like testosterone. When elevated in women they can cause acne, thinning hair, undesirable hair growth on the face, chest or back, and oily skin.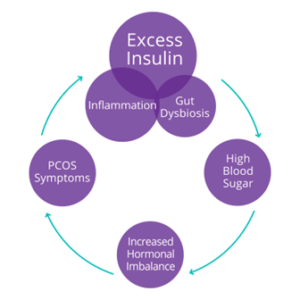
People with PCOS usually have high levels of androgens because they also have increased luteinizing hormone (LH) levels. LH plays an important role in regulating the menstrual cycle and triggering the release of an egg from the ovaries. When these hormones are not in balance, it causes menstrual irregularities, making it harder for people with PCOS to get pregnant.
Another reason for a rise in androgen levels is an increase in insulin levels. That’s because high levels of insulin cause the ovaries to make and release more androgens, ultimately suppressing ovulation and leading to problems with fertility.
The insulin connection
Most individuals experiencing PCOS have some level of insulin resistance, which is often a result of diet and lifestyle. Insulin is a hormone made in the pancreas that plays a major role in helping the body extract glucose from the bloodstream to use as energy. Insulin resistance occurs when your cells don’t respond well to the hormone insulin and can’t use glucose in the blood as an energy source, leaving levels high in the bloodstream.
Chronically elevated insulin levels have been linked to higher androgen production. Elevated androgens cause ovulation to slow down, increasing the chance of ovulation becoming irregular or stopping completely. This is what leads to the accumulation of follicles in the ovaries.
Under healthy circumstances, follicles mature and are released through ovulation, and remaining follicles disintegrate in the ovaries. In cases of PCOS, imbalanced hormones block the ovaries from being able to fully develop follicles to maturity so they can accumulate. This is why a common symptom of PCOS is irregular periods accompanied by low ovulation and difficulty getting pregnant.
Managing PCOS
Prioritizing a nutritious diet and living a healthy lifestyle are the most impactful changes you can make to improve all symptoms including restoring your period, improving fertility and reducing high levels of androgens.
Creating new eating habits
One of the best things you can do for your body is to eat a variety of nutrient dense foods, giving it the fuel it needs for important functions like creating hormones and maintaining a regular menstrual cycle. There is no specific diet that has been shown to be the frontrunner for supporting PCOS. But, a diet that is centered around whole foods and high quality protein sources will be supportive of restoring your body’s balance.
Balancing blood sugar is also a helpful focus when it comes to making changes to your diet. This will not only normalize insulin, but indirectly lower androgens. This happens because once insulin levels are no longer elevated, ovarian function can also be restored which means lower androgens. Try creating new eating habits instead of following an overly restrictive diet that eliminates specific food groups.
Here are some helpful eating habits to keep in mind:
- Always eat carbohydrates with protein and fat
- Eat every 3-4 hours to maintain blood sugar levels
- Eliminate highly processed foods, like pastries, cakes, candy, crackers
- Reduce intake of bread and grains
Exercising for PCOS
Since PCOS often goes hand in hand with insulin resistance, increasing the body’s sensitivity can help manage PCOS symptoms at the root.
Insulin acts as a fat storage hormone. When cells don’t respond to insulin, glucose can’t get into the cell and it’s stored as fat. This is why PCOS can lead to weight gain, and make weight loss more difficult. Exercise improves the ability of muscles to take up glucose, which in turn lowers insulin levels. Practiced regularly, this has a positive effect on overall insulin sensitivity.
Forms of exercise that are most beneficial include strength or resistance training because they help to build muscle. Increased muscle mass improves insulin levels by increasing the overall function of the cell, including its sensitivity to insulin, while also increasing metabolism. However, any exercise that feels good for you is better than no exercise when it comes to PCOS. Find something that you like doing, and make it part of your daily routine.
Supporting hormonal imbalance
Diet and exercise can be game changers for improving your PCOS symptoms, but adding supplementation can create an even more powerful approach. As we’ve seen, insulin resistance may not directly cause PCOS, but there is a strong association with its development.
Inositols, a type of sugar produced naturally in the body, have the ability to impact PCOS. In particular, myo-inositol and D-chiro-inositol. Myo-inositol is converted to D-chiro-inositol to aid glucose metabolism under healthy circumstances. But, insulin resistance can hinder this action.
Supplementation with D-chiro-inositol has been shown in numerous studies not only to reduce insulin and testosterone levels but also improve menstrual regularity, ovarian function, and egg quality. You can try adding a supplement like PCOS Pro Ultra Relief to help alleviate your PCOS symptoms. This formula contains 600mg of D-chiro-inositol and is designed to provide relief from PCOS symptoms, help normalize menstrual cycle irregularities, and promote healthy ovulation.
Living with PCOS is no picnic, but there are many things you can do to support your body and restore balance. When armed with the right tools and strategies like diet, exercise and supplementation, you can be better prepared to tackle PCOS symptoms.
The information in this article is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of a qualified health professional regarding any questions about your medical condition. Do not disregard professional medical advice or wait to seek advice or treatment because of something you have read here.
Sources:
Hawley, J.A., & S.J. Lessard (2008). Exercise training-induced improvements in insulin action. Acta Physiologica, 192(1), 127-135.
Kalra, B., Kalra, S. & J.B. Sharma (2016). The inositols and polycystic ovary syndrome. Indian Journal of Endocrinology and Metabolism, 20(5,) 720-724.
Lujan M., Chizen D., Pierson R. (2008). Diagnostic criteria for polycystic ovary syndrome: pitfalls and controversies. J Obstet Gynaecol Can. 2008 Aug;30(8):671-679.
Rasquin Leon LI, Anastasopoulou C, Mayrin JV. Polycystic Ovarian Disease. [Updated 2022 May 9]. In: StatPearls. Treasure Island (FL): StatPearls Publishing.
Insulin resistance: What is it and how does it contribute to diabetes and weight gain
Everything You Need to Know About Insulin
Polycystic Ovary Syndrome (PCOS)
Patient education: Polycystic ovary syndrome (PCOS) (Beyond the Basics)